Swelling in the legs and feet can be a sign of something serious
By Wendy Haaf
Photo: iStock/Marina113.
Swelling in the feet and legs, while often benign, can sometimes herald a potentially life-threatening medical emergency or a serious systemic disease. Even when the underlying cause is relatively innocuous, if that puffiness—known medically as “edema”—persists, it can increase the chance of experiencing problems such as skin ulcerations and slowed wound healing. Here’s what you need to know about when to seek medical attention for lower-limb swelling and what you can do to reduce or minimize chronic edema.
What’s Happening?
Let’s first explore how edema can occur.
“We think of blood vessel walls as being solid, but they’re not,” notes Dr. Lee Green, a professor and the chair of the Department of Family Medicine at the University of Alberta’s Faculty of Medicine and Dentistry in Edmonton. “They’re kind of porous, and fluid from the watery part of the blood can leak out of them pretty easily” and collect in the spaces between cells. Because the lymphatic system—which is responsible for returning this fluid in the direction of the heart—is mostly working against gravity, this can occur on a minor scale, say, if you stand for an extended period. But certain abnormalities can allow large amounts of fluid to escape or to interfere with the system’s normal functioning, thereby trapping fluid in the feet and legs.
One of the least common but most imminently worrisome possible causes of such swelling is deep-vein thrombosis (DVT), a condition in which a clot forms within one of the blood vessels, blocking normal blood flow and causing fluid to back up into the surrounding tissue. The danger here is that a piece of the clot will break off and travel to the lungs, brain, or heart and cause a life-threatening stroke or pulmonary embolism.
Next on the list of relatively uncommon but consequential possible causes is organ failure. Dr. Henry Yu-Hin Siu, an assistant professor and the director of the Enhanced Skills: Care of the Elderly program in the Department of Family Medicine at McMaster University in Hamilton, ON, explains how faltering function of the heart, liver, or kidneys can lead to edema. Normally, “fluid stays within a blood vessel for two reasons,” he says. “One, the pressure inside the vessel isn’t enough to push the fluid out. Two, the concentration of the proteins—or what we call the ‘solutes’—in the blood vessel is high enough to keep the water inside.
“When either of those forces is a bit off—for example, in the case of congestive heart failure, when the pressure is higher because the heart is not pumping as effectively as it should—the fluid is being pushed out of the blood vessel,” Siu says. “In the case of something like liver failure, the body is not making enough proteins to keep the fluid inside, so the fluid leaks out of the blood vessel.” Malfunctioning kidneys can hinder the elimination of fluid (thereby boosting pressure in the blood vessels), while damage to these organs’ filtering units can allow proteins to pass into the urine rather than remaining in the blood; if blood-protein levels fall sufficiently low, fluid escapes from the vessel.
The three factors to remember when you’re wondering whether to seek medical attention for edema—and if so, how urgently—are how quickly it comes on, whether it affects one or both sides of the body, and the presence or absence of other symptoms.
If you experience swelling on one side only that evolves rapidly over a day or two, particularly if it’s accompanied by redness, tenderness, or pain in the leg—which hint at possible DVT—you should see your doctor sooner rather than later. “Absolutely try to get in within the day, if possible,” Siu says.
You should also seek immediate medical attention if you experience unilateral swelling accompanied by shortness of breath (a symptom that can result from a clot in the lungs) during everyday activities such as gardening and housework. (Depending on the pattern of symptoms, certain tests—such as a Doppler ultrasound to look for blood clots in the leg—can be used to confirm or rule out suspected DVT. If it turns out that you have DVT, but you don’t have any risk factors—such as smoking or a family history of blood clots—a second set of tests may be recommended. Since some cancers can change your metabolism in a way that increases clot risk, “if you develop a blood clot out of the clear blue and you’re 60 years old,” the University of Alberta’s Dr. Green says, “your doctor may want to do some basic investigations to make sure you don’t have a lung tumour or a bowel tumour or something like that.”
While not as urgent, new and persistent swelling on both sides of the body that comes on in less than a week is worth getting checked out fairly promptly—say, within a few days. Here, too, doctors look for other symptoms to help narrow the list of suspects.
“In the case of the heart, I would be asking, ‘Are you more short of breath during daily activities—gardening, doing your laundry, going up and down the stairs—that you had no problem doing before?’” Siu notes. “Other questions I would probably ask are, ‘How are you sleeping at night? Are you finding you need to prop up your head with multiple pillows, or more so than before?’” These things, in conjunction with bilateral leg swelling, point towards possible heart failure. In such cases, a blood test called a BNP, a chest X-ray, and possibly an echocardiogram—a type of ultrasound that measures heart function—would be warranted.
On the other hand, if two-sided edema is your sole symptom, your doctor may look at your medical history for other clues, such as a new prescription (edema can be a side effect of certain drugs, such as amlodipine, which is used to treat high blood pressure), a history of liver disease or past heavy alcohol use (risk factors for liver failure), and poorly controlled diabetes (which can lead to kidney failure). With the exception of the medication reaction, the workup for any of these problems starts with blood tests.
Walk, Walk, Walk
Most of the time, however, edema is due to more mundane causes, such as pooling of blood in the lower legs due to valves in the blood vessels (imagine doors that are supposed to open only in one direction) becoming faulty or leaking.
Assuming this is the case, what can you do to manage or minimize swelling? If you’re carrying around excess weight (which exerts extra pressure on your blood vessels and lymphatic system), you could try improving your lifestyle by cutting back on processed foods and eating more fruits and vegetables. (Even if you don’t lose a few kilos, this strategy will cut the amount of sodium in your diet, which itself helps by reducing water retention.) Elevating your legs above your heart when you’re resting, reading, or watching television may also be useful.
By far the most powerful tool, however, is walking. When you put one foot in front of the other, the muscles in your calf act like a second heart, squeezing and pumping fluid back upward, notes Pamela Houghton, a professor in the Department of Physiotherapy and the chair of the MCISc (Advanced Health Care Practice) program at Western University in London, ON. “I say to people, ‘Walk, don’t stand,’” she says. (If your mobility is severely limited or you want to augment walking, while seated, you can pump your ankles back and forth as if driving a car, Siu suggests.)
Since a rolling heel-to-toe stride helps the “calf-muscle pump” function optimally, if you are able to take only short, shuffling steps, or if you walk slowly or with a limp, Houghton recommends consulting a physiotherapist. For your leg muscles to be strong enough to pump fluid effectively, “you need to have a certain flexibility in your ankle,” she explains, adding that a physiotherapist can assess your gait and, if necessary, prescribe various exercises to increase the flexibility of the joint and strengthen your calf muscles.
Used in conjunction with walking, garments called compression stockings can also be very effective for minimizing swelling. Now available in a rainbow of colours and styles from athletic-supply stores (many pharmacies carry plainer, more budget-conscious options), these hose help prevent fluid from collecting in the legs.
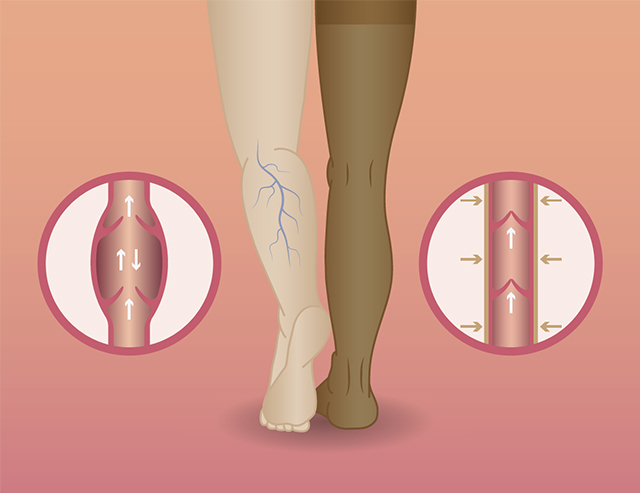
Illustration: iStock/Antaya.
Two caveats before you buy. Siu recommends first getting the okay from your doctor, noting that, for example, if you don’t have sufficiently robust blood flow in your lower legs, compression stockings could cut off your circulation. You should also hold off if you’re going to see a physiotherapist: since during active treatment, legs may shrink more than one hose size, bandages are sometimes used until the swelling stops. In that scenario, “If you start with stockings, they’ll just end up sagging,” Houghton says.
Ideally, you should don the hose before you even get out of bed, when edema is at its lowest level, leaving them on until the end of the day, if possible (though admittedly, this can be difficult during hot, humid weather). “That will minimize the amount of new swelling that you accumulate throughout the day,” Siu says.
Siu also recommends regularly applying moisturizing cream or lotion to your lower legs and feet to prevent the skin from drying out and cracking. (And, “if you have swelling to the point that it’s causing red, itchy patches on the legs, see a doctor,” he adds. “There are medicated creams we can provide to calm that down and keep skin integrity as strong as possible, which will help prevent wounds in the future.”)
If you think of these measures as pleasurable self-care rather than a chore, they’ll lift your spirits in addition to improving your day-to-day comfort.