There’s no one-size-fits-all plan, but diet and exercise are key
By Caitlin Finlay
With Type-2 diabetes, the body either doesn’t produce enough of the hormone insulin to regulate the amount of sugar in the blood or isn’t able to use effectively the insulin it does produce. The disease is commonly developed in adulthood but can also affect children. Diabetes causes dangerous fluctuations in blood-sugar levels and increases the risk for other problems such as heart attack, stroke, kidney disease, and eye disease. Managing the disease involves regular exercise, maintaining a regular diet, and medication or insulin therapy as needed. While there’s no one-size-fits-all course of action, there are recommendations that can help.
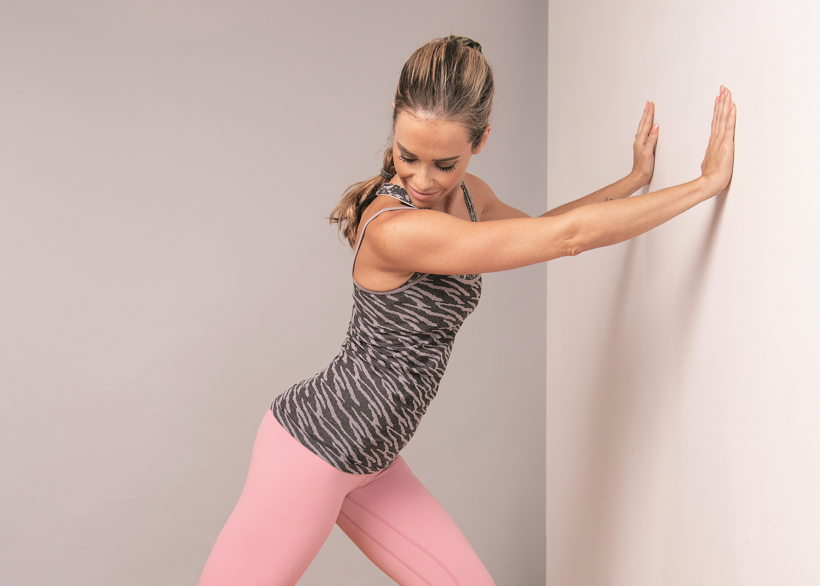
Exercise:
Most of us dread exercise, but it’s especially important in managing diabetes. Physical activity helps to lower blood-sugar levels, decreases the risk for heart disease, improves blood pressure, reduces stress, and promotes weight loss.
Both aerobic and resistance exercises are recommended for those with diabetes. Aerobic exercises include cycling, going for a brisk walk, and jogging. Resistance exercises include weight training or body weight exercises; to prevent strain or injury, it’s important to have the proper form doing these types of exercises. If you’re new to exercising, be sure to discuss it with your doctor, start slow, monitor your blood sugar before, during, and after your workouts, and carry a snack with you in case your blood sugar drops too low.
Diet:
The goal when it comes to a Type-2 diabetes diet is managing blood sugar, weight, blood pressure, and cholesterol, and reducing the risk for complications. All of this can sound daunting, but there are many resources available to help.
Diabetes Canada recommends eating regular meals, no more than six hours apart, three times a day. Ideally, meals should be eaten at about the same time each day to maintain blood-sugar levels. You should also aim to eat approximately the same sized meals—don’t have a big breakfast and a small lunch, for example.
If you’ve recently been diagnosed with Type-2 diabetes or are at risk and want to make dietary changes, remember that it’s a process and should be done gradually. Introduce one or two changes at a time, integrate those changes into your routine, and then consider introducing an additional one or two changes.
The main things to consider when managing a diabetes-friendly diet are carbohydrates, portion size, and meal planning.
Because our bodies process carbohydrates as sugars, carbs will affect your blood-sugar level, especially so when you’re on certain medications. However, not all carbohydrates are bad. “Good” carbohydrates include whole grains, vegetables, fruits, and legumes. Good carbs can lower your risk for heart disease and stroke, and leave you feeling full longer; in addition, they have a low glycemic index, meaning that they won’t increase your blood sugar too much. Nevertheless, portion size still matters, and counting carbs—monitoring your carbohydrate intake—is a common strategy.
Canada’s Food Guide recommends that half of your plate consist of fruits and vegetables; for those with diabetes, though, it should be mainly vegetables because they have less sugar than fruits. The rest of the plate should be evenly split between proteins and whole grains.
As a “handy” guide, Diabetes Canada recommends that portions of grains, starches, and fruits be about the size of your fist. If you love vegetables, you’re in luck because you can eat as much as you can fit in both hands. For meat and alternatives, Diabetes Canada recommends a portion the size of the palm of your hand and the thickness of your little finger. Fat should be limited to an amount the size of the tip of your thumb.
Planning meals and snacks in advance is the best way to avoid eating foods that will increase your blood sugar. The best foods to eat, whenever possible, are whole foods prepared at home. Whole foods are those that aren’t processed and don’t have the sodium, saturated fats, and sugars that are often added to processed foods. A good example is fruits versus fruit juices: while both contain some sugar, fruit juices and juice concentrates have a lot of sugar added to them. Most beverages are processed and have added sugars, so your best option for quenching your thirst is good old water.
With all these recommendations, planning meals can quickly become overwhelming, but there are lots of resources available for you. To get you started, we’ve included a list of resources and recipes below.
(Please note: these resources and recommendations do not replace the personalized advice a doctor or dietician can provide. If you have diabetes or simply want to make dietary changes, it’s best to consult a doctor or dietician.)
Resources:
Meal planning tips for women: https://www.unlockfood.ca/getmedia/33be5a0c-b53a-48d1-a293-311a7f723b18/Type-2-Diabetes-Menu-Plan-Female-July-2018.aspx
Meal planning tips for men: https://www.unlockfood.ca/getmedia/49c06154-3b49-48ba-92e3-465eaa5a10ca/Type-2-Diabetes-Menu-Plan-Male-July-2018.aspx
A list of sweeteners and their affects on blood sugar: https://diabetes.ca/DiabetesCanadaWebsite/media/Managing-My-Diabetes/Tools%20and%20Resources/sugars-and-sweeteners.pdf
Recipes:
Photo: iStock/Milaspage.